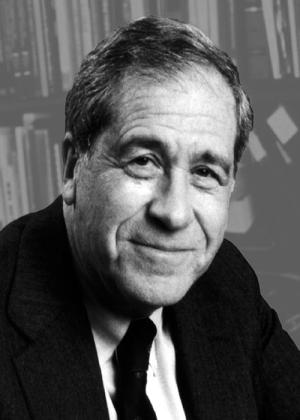
Bernard Fisher, M.D., set out to understand the biology and development of breast cancer before The National Cancer Act was even signed in 1970. He believed in clinical research and insisted that data driven medical decisions. Data from one of his treatment trials led to a breakthrough in cancer prevention, a drug that cut breast cancer risk in half for women at increased risk.
NSABP B-14 was a study of tamoxifen vs. placebo in women with early stage, node-negative, estrogen receptor positive breast cancer. The participants had small tumors removed by surgery and then received tamoxifen or a placebo daily for 5 years. Women in the tamoxifen group had better disease-free survival and fewer new cancers in their opposite breast.
If tamoxifen could prevent new cancers in these women, who were known to be at increased risk of getting a second, new breast cancer, why not test the drug in women at increased risk of breast cancer who had not yet gotten the disease? The National Cancer Institute extended an invitation to all the NCI sponsored research networks to come up with a study to test the idea that tamoxifen given to postmenopausal women at increased risk of breast cancer could reduce their risk.
Dr. Fisher’s research group, the National Surgical Adjuvant Breast and Bowel Project (NSABP), was chosen to lead the trial, and successfully justified including premenopausal women. Hearings at the U.S. Food and Drug Administration and in Congress preceded the trial’s opening, as many officials were concerned about using a treatment drug in healthy, high-risk women.
The trial opened in 1992. On March 24, 1998, an independent data-monitoring committee determined that the finding indicated a reduction in breast cancer risk sufficiently strong to disclose the results and permit women receiving placebo an opportunity to take tamoxifen. Women taking tamoxifen had almost 50 percent fewer breast cancers in all age groups and all levels of risk.
To learn more about Dr. Fisher, read this article in Cancer Research.