“In God we trust, all others must have data.” Bernard Fisher, M.D.
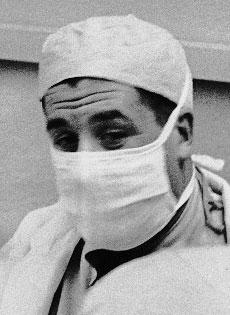
Bernard Fisher, M.D., a surgeon at the University of Pittsburgh, firmly believed in the scientific process and data-driven decisions. In 1957, he was invited to a meeting about breast cancer at the National Institutes of Health. He found little information on the biology of breast cancer and a lack of researcher interest in understanding the disease. So, he gradually shifted his research from transplantation biology and liver regeneration to breast cancer.
Collaborating with his brother on laboratory and animal studies to understand how breast cancer spread in the body, he found cancer cells reached the bloodstream early in the disease. This went against the prevailing idea that cancer spread out in areas adjacent to the tumor. (This finding also helped him to pioneer adjuvant therapy to kill the cancer cells in the bloodstream after surgery.)
He believed that the prevailing surgery of the late 1950s–radical mastectomy, removing the breast, lymph nodes, chest muscles, and sometimes bones of the chest–made no sense. He had seen cancer cells in the bloodstream early in the disease, which went against the idea that cancer spread out in areas directly adjacent to the tumor. The radical surgery also left women disfigured and weakened, with swollen arms from lack of lymph nodes and difficulty moving their arm from the loss of chest muscle. By 1967, he was chairman of the National Surgical Breast and Bowel Project (NSABP), a major network of researchers in breast and colon cancer treatment, headquartered in Pittsburgh, PA. One of the first breast cancer studies done by the group was a trial of different surgeries begun in August 1971: radical mastectomy, simple mastectomy (removal of the breast only), or simple mastectomy plus radiation treatment.
NSABP B-04, as the trial was numbered, was anathema to many surgeons, who considered any surgery less than radical mastectomy to be malpractice. When the results were published in 1977, women who had radical mastectomies suffered disability and disfigurement and lived no longer than women who received simple mastectomies. Thus began the shift away from debilitating radical surgeries to techniques that preserved the breast and the functioning of patients with cancer.
Read the 25-year follow up to the NSABP B-04 trial in The New England Journal of Medicine.